Addison’s disease, also called hypoadrenocorticism, is a disorder in which the adrenal gland does not produce sufficient hormones. The adrenal  glands are essential for life. When the adrenal gland fail, the consequences are very severe.
glands are essential for life. When the adrenal gland fail, the consequences are very severe.
What are the missing hormones in Addison's disease?
Dogs with hypoadrenocorticism (Addison's disease) are unable to produce one or two steroid hormones, both secreted from the adrenal cortex (outer layer of the adrenal gland).
The first hormone that's missing is cortisol, which is very important in maintaining a normal metabolism, as well as a general sense of well being.
The second hormone that's missing is aldosterone, which manages the water balance and serum electrolytes in the body.
What are the different forms of hypoadrenocorticism?
Hypoadrenocorticism can be divided into primary and secondary subtypes.
- With primary hypoadrenocorticism (Addison's disease), the problem lies in the adrenal gland itself, with atrophy or destruction of the gland.
- With secondary hypoadrenocorticism, the adrenal gland are normal, and the problem lies in the pituitary gland. The pituitary gland normally secretes a hormone called ACTH (adrenocorticotropic hormone) that stimulates the adrenal gland to secrete its hormones; in secondary hypoadrenocorticism, ACTH is not secreted in needed amounts, leading to the secondary adrenal insufficiency.
What causes Addison's disease in dogs?
In most dogs, we cannot determine what caused their adrenal disease. With primary hypoadrenocorticism, the following causes must be considered.
- Most dogs with the primary form appear to have an autoimmune condition in which the body destroys part of the adrenal cortex
- Very rarely, infiltrative conditions such as cancer can metastasis to and destroy the adrenal gland to cause Addison’s disease
- Occasionally, treatment of Cushing’s disease with the drugs mitotane and trilostane will result in complete adrenal destruction and Addison’s disease
With secondary hypoadrenocorticism, we must rule out the following underlying causes.
Congenital deficiency of ACTH secretion
Pituitary tumors, inflammation or trauma that have destroyed most of the ACTH-secreting cells in the pituitary gland, leading to deficient ACTH secretion
Are some dogs predisposed to developing this disease?
Although hypoadrenocorticism can develop in any age, breed, or sex of dogs, the following points should be taken into consideration when making a diagnosis.
- Hypoadrenocorticism is most common in young to middle-aged dogs.
- Most dogs with Addison's disease are females.
- Bearded Collies, Standard Poodles (see photo on left, below) , Great Danes, Portuguese Water Dogs, West Highland White Terriers (see photo on right, below), and Leonbergers are all predisposed to developing this disease.


Chain of events leading to severe hypoadrenocorticism in dogs
With primary hypoadrenocorticism (Addison's disease), the dog generally develops complete adrenocortical destruction with both cortisol and aldosterone deficiencies.
Aldosterone is the main mineralocorticoid hormone, and it affects the levels of potassium, sodium, and chloride in the blood. Low levels of aldosterone cause potassium to gradually build up in the blood and, in severe cases, cause the heart to slow down or beat irregularly. Some dogs have such a slow heart rate (50 beats per minute or lower) that they can become weak or go into shock.
Less commonly, dogs will develop secondary or "atypical” primary hypoadrenocorticism. This subgroup of dogs are only deficient in cortisol and appear to maintain a normal aldosterone level, at least early in the course of their disease. These dogs are more difficult to diagnose because their signs are milder and the serum potassium, sodium, and chloride values all remain normal.
Clinical features of hypoadrenocorticism in dogs
Historically, hypoadrenocorticism generally has a waxing and waning course and may be confused with other diseases because the clinical signs are not specific. The most common clinical signs and physical exam finding include the following:
- Depression or lethargy
- Weakness or collapse
- Anorexia (poor appetite)
- Weight loss
- Vomiting or diarrhea
- Excessive thirst and urination
- Hypothermia (low body temperature)
- Dehydration and shock
Signs of Addison’s disease include repeated episodes of vomiting and diarrhea, loss of appetite, dehydration, and gradual, but severe, weight loss. Because the clinical signs of Addison’s disease are vague and nonspecific, it can be difficult to diagnose in the earlier stages of disease. Therefore, severe consequences, such as shock and evidence of kidney failure, can develop suddenly in some dogs.
In my next post, I'll discuss how we can diagnose and treat hypoadrenocorticism, can will be fatal if not properly managed.
Źródło: nimalendocrine.blogspot.com
The growing concern surrounding the release of radiation from an earthquake and tsunami-stricken nuclear complex in Japan has raised fears of radiation exposure to populations in North America from the potential plume of radioactivity crossing the Pacific Ocean.
Because I use radioactive materials both to treat cats with hyperthyroidism (radioiodine; I-131) and to perform nuclear imaging procedures (ie, thyroid, bone, renal, liver scans— see my website for more information), many veterinarians have contacted me with questions and concerns.
Over the weekend, the American Association of Clinical Endocrinologists, the American Thyroid Association, The Endocrine Society and the Society of Nuclear Medicine issued a joint statement written to help Americans understand their radiation-related health risks. I thought that many of you might find this helpful in understanding the situation and what you and your family should know.
RADIATION RISKS TO HEALTH:
A Joint Statement from the American Association of Clinical Endocrinologists, the American Thyroid Association, The Endocrine Society and the Society of Nuclear Medicine March 18, 2011
Chevy Chase, MD (March 18, 2011)--The growing concern surrounding the release of radiation from an earthquake and tsunami-stricken nuclear complex in Japan has raised fears of radiation exposure to populations in North America from the potential plume of radioactivity crossing the Pacific Ocean. To help Americans understand their radiation-related health risks, the American Association of Clinical Endocrinologists (AACE), the American Thyroid Association (ATA), The Endocrine Society and the Society of Nuclear Medicine (SNM) issued a joint statement.
The statement suggests that the principal radiation source of concern, in regard to impact on health, is radioactive iodine including iodine-131.This presents a special risk to health because exposure of the thyroid to high levels may lead to development of thyroid nodules and thyroid cancer years later.
Radioactive iodine uptake to the thyroid can be blocked by taking potassium iodide (KI) pills. However the statement cautions KI should not be taken unless there is a clear risk of exposure to high levels of radioactive iodine. While some radiation may be detected in the United States as a result of the nuclear reactor accident in Japan, current estimates indicate radiation levels will not be harmful to the thyroid gland or general health. If radiation levels did warrant the use of KI, the statement recommends it should be taken as directed by physicians or public health authorities until the risk for significant exposure dissipates.
The statement discourages individuals needlessly purchasing or hoarding of KI in the United States. Since there is not a radiation emergency in the United States or its territories, the statement does not support the ingestion of KI prophylaxis at this time. KI can cause allergic reactions, skin rashes, salivary gland inflammation, hyperthyroidism or hypothyroidism in a small percentage of people.
The American Association of Clinical Endocrinologists, American Thyroid Association, The Endocrine Society and the Society of Nuclear Medicine will continue to monitor potential risks to health from this accident and will issue amended advisories as warranted.
Źródło: endocrinevet.blogspot.com
However, by following the protocol outlined below, you can easily dilute, aliquot and store Cortrosyn after reconstitution for up to 6 months. This makes each ACTH stimulation test much less expensive, because each vial of Cortrosyn can be used to perform as many as five ACTH stimulation tests.
 Cortrosyn is supplied in vials each containing 0.25 mg (250 µg) of synthetic ACTH (cosyntropin) in powder form. Because the dose of Cortrosyn used to perform an ACTH stimulation test is only 5 µg/kg, small to medium sized dogs require only a fraction of the ACTH contained in each vial.
Cortrosyn is supplied in vials each containing 0.25 mg (250 µg) of synthetic ACTH (cosyntropin) in powder form. Because the dose of Cortrosyn used to perform an ACTH stimulation test is only 5 µg/kg, small to medium sized dogs require only a fraction of the ACTH contained in each vial.For more information on how to perform an ACTH stimulation test, see my post entitled, What's the best protocol for ACTH stimulation testing in dogs and cats?
How to aliquot and store each vial of Cortrosyn for subsequent use? It's simple — just follow the directions outlined here:
1. Reconstituted the Cortrosyn power by adding exactly 2.5-ml of sterile saline solution to the vial. With this dilution, the resulting concentration of the Cortrosyn solution in the vial would be 100 µg /ml.
2. Once Cortrosyn is reconstituted, aspirate 50-µg doses (0.5 ml) into 5 plastic syringes. Or, if smaller ACTH doses are desired, aspirate 25-µg doses (0.25 ml) into 10 syringes. (For more accurate dosing, I use insulin or tuberculin syringes).
DO NOT store reconstituted Cortrosyn in glass containers or vials. The reason that the Cortrosyn needs to be stored in plastic is that ACTH will stick to glass, thereby lowering the available amount of Cortrosyn that would be injected at time of testing.
3. The syringes containing the reconstituted, diluted Cortrosyn should be labeled with the product, dose in each syringe, and the date the Cortrosyn was reconstituted.
4. Freeze each of the syringes at -20oC. Avoid storing these syringes in a frost-free freezer, which must periodically warm up to de-frost. Repeated freezing and thawing cycles would compromise the integrity of the Cortrosyn.
When frozen properly, aliquots can be stored for up to 6 months without loss of efficacy.
5. Alternatively, the Cortrosyn solution can be stored refrigerated (4oC) where it has been shown to be bioactive and stable for at least 4 weeks.
Diluting the Cortrosyn and using a low-dose ACTH stimulation test protocol is very cost-effective. In this way, 1 vial of Cortrosyn can be used to test multiple patients without compromising the quality of the test results.
As an example, at the 5-µg/kg dose, 5 dogs weighing 10 kg (22 lbs) can be tested using a single vial, reducing the cost of the drug by 80%. By looking at the cost benefit, it is clear that the savings could be significant by using this testing protocol.
Źródło: endocrinevet.blogspot.com
We are trying to concur on choice of the single best test to screen cats for hyperthyroidism. Is determination of total T4 still the gold standard for screening the majority of cats?
My Response:
 Use of a serum total T4 concentration is absolutely the best single screening test. But remember, the diagnosis of hyperthyroidism can never be based on a single total T4 alone. It has to be based on the presence of clinical features (eg. weight loss despite a good appetite) together with the presence of a thyroid nodule. If many clinical signs of hyperthyroid are present in a cat with a high total T4 but a thyroid nodule is not palpable, it's always a good idea to confirm the diagnosis by repeating the T4 and/or measuring a free T4 concentration.
Use of a serum total T4 concentration is absolutely the best single screening test. But remember, the diagnosis of hyperthyroidism can never be based on a single total T4 alone. It has to be based on the presence of clinical features (eg. weight loss despite a good appetite) together with the presence of a thyroid nodule. If many clinical signs of hyperthyroid are present in a cat with a high total T4 but a thyroid nodule is not palpable, it's always a good idea to confirm the diagnosis by repeating the T4 and/or measuring a free T4 concentration.
In some cats with mild hyperthyroidism, the total T4 can be high-normal or only borderline high. In these cats, a free T4 measurement is commonly used to help verify the diagnosis. The free T4 value should NEVER be run without a total T4; the specificity of the T4 is quite poor, and many cats without hyperthyroidism will have a high free T4 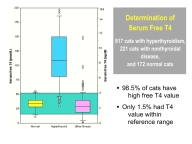 concentration. Therefore, the presence of a high free T4 with a normal T4 is not really diagnostic for hyperthyroidism unless the cat is showing clinical signs of the disease and has a palpable thyroid nodule.
concentration. Therefore, the presence of a high free T4 with a normal T4 is not really diagnostic for hyperthyroidism unless the cat is showing clinical signs of the disease and has a palpable thyroid nodule.
 Again, without clinical features and physical exam findings consistent with hyperthyroidism, it's always best to wait and retest at 1-3 month intervals. Thyroid scintigraphy (see Figure on left) can also be a very helpful diagnostic aid in these cats. Cats with mild hyperthyroidism have an increased uptake of the radionuclide by their thyroid nodules. The percent uptake (or thyroid:salivary ratio) can be calculated and used as a sensitive diagnostic test for hyperthyroid cats.
Again, without clinical features and physical exam findings consistent with hyperthyroidism, it's always best to wait and retest at 1-3 month intervals. Thyroid scintigraphy (see Figure on left) can also be a very helpful diagnostic aid in these cats. Cats with mild hyperthyroidism have an increased uptake of the radionuclide by their thyroid nodules. The percent uptake (or thyroid:salivary ratio) can be calculated and used as a sensitive diagnostic test for hyperthyroid cats.
Sound difficult? Unfortunately, it is not always so easy to correctly diagnose hyperthyroidism in cats. But remember that treatment of hyperthyroidism is never an emergency, especially if the hyperthyroidism is very mild. If a 'borderline' cat does have hyperthyroidism, the thyroid nodule will grow and the total T4 will become high with time.
Źródło: endocrinevet.blogspot.com
About a month ago, I posted that the Diagnostic Center for Population and Animal Health (DCPAH) at Michigan State University had announced that the reagents for their parathyroid hormone related protein assay (PTHrP) were not longer available.
This week Michigan State University's DCPAH announced that they are back in business and can again run serum samples for both parathyroid hormone (PTH) as well as PTHrp.
This is the only laboratory that offers the PTHrp test used in the workup for dogs and cats with hypercalcemia. So this is great news that this important assay is up and running again soon.
See the Announcement page on the DCPAH website for more information.
Źródło: endocrinevet.blogspot.com
Due to an inventory error, we have found ourselves with 3 bottles of synthetic ACTH (Cortrosyn) that have an expiration date of a month from now. Would you recommend reconstituting all 3 vials and freezing into aliquots at this point? Before I throw out several hundred dollars worth of Cortrosyn, I wanted to ask you opinion.
Additionally, for future use, what is the current dosing recommendation when using previously reconstituted Cortrosyn? Are there special considerations for freezing it?
Thanks so much for your help.
My Response:
Officially, I cannot condone the use of drugs past their expiration date, but it makes some sense to me that if you reconstitute it and freeze it now, that you could keep the aliquots for 6 months. The problem is if you get results that you weren't expecting (ie, lower than expected ACTH-stimulated cortisol values), then you have to question whether the Cortrosyn is still potent, but I'd suspect it will be okay.
If it was still in date, you could try selling some to neighboring clinics, but I'm not so sure you can or should do that with expired drug.
Click here to see my previous post about how I recommend reconstituting and freezing Cortosyn for future use. And click here to see my post on the best dose to use for ACTH stimulation testing.
Źródło: endocrinevet.blogspot.com
'm treating a 10-year old, F/S Bichon Frise who has been on 2.5 mg of prednisone daily for months. Her appetite has always been good, but recently she has become extremely ravenous on the same dose of prednisone. In addition, lately she has become noticeably more polyuric and polydipsic (PU/PD).
So, I suspect that naturally-occurring Cushing's syndrome may be developing — oddly, while taking predisone. We found not abnormalities on her routine lab work except an very high serum alkaline phosphatase activity of 1100 U/L (reference range < 100 U/L).
My thought is that stopping the predisone for a few days should be enough to allow for us to perform an ACTH stimulation test or a low-dose dexamethasone suppression test (LDDST). That amount of time will allow the predisone to leave the system so there won't be any interference with the testing. It would seem to me that an interval longer than a few days shouldn't be needed.
That being said, everyone keeps telling me it will take a few months for the adrenals to regenerate once I stop the prednisone. Presuming this dog has truly developed PDH or an FAT, does it make any sense to you that I should have to wait any longer than just a few day to let the prednisone out of the body?
My Response:
Good question. If this dog's pituitary and adrenal glands are "normal" (ie, she does not have naturally occurring Cushing's disease - either pituitary-dependent hyperadrenocorticism or a functional adrenal tumor), then the prednisone could feedback on the dog's normal pituitary gland to inhibit ACTH secretion. With time, the resulting low circulating ACTH concentrations would lead to atrophy of the inner 2 zones of the adrenal gland that secrete cortisol.
If you stop the prednisone for 24-48 hours and do an ACTH stimulation test in that dog, the results would likely show a low to low-normal basal cortisol with a "blunted" cortisol response to ACTH stimulation (generally > 2.0 ug/dl but < 6 ug//dl). Despite the suppression basal and ACTH-stimulated cortisol values, that same dog with iatrogenic hypoadrenocorticism could show clinical signs of iatrogenic hyperadrenocorticism (due to the direct glucocorticoid effects of the prednisone).
Now, if this dog really does have natural Cushing's syndrome (either pituitary-dependent hyperadrenocorticism or adrenal tumor), the doses of prednisone you are giving will NOT be high enough to shut off pituitary ACTH secretion or suppress adrenal cortisol section. (This "resistance" to glucocorticoid negative feedback in Cushing's disease is the whole physiologic basis for use of the low-dose dexamethasone suppression test.).
So in this dog with Cushing's syndrome, performing an ACTH stimulation test after being off the prednisone for 24-48 hours would show a normal to high basal cortisol with a high-normal to exaggerated serum cortisol response. In other words, the prednisone would not affect the ACTH stimulation test because the adrenal cortex would still be hypertrophied.
Another important point: in this scenario, you want to use and ACTH stimulation test, not the low-dose suppression test. If another long discussion for me to explain the reason why that's the case, but you can get false-positive results in dogs with iatrogenic Cushing's disease so you do NOT want to use a low-dose dexamethasone suppression test in this dog, at least as your initial test.
Źródło: endocrinevet.blogspot.com
Buster is overweight at 17 pounds, but he has lost 3 pounds on a weight loss plan. Other than being overweight and increased bronchovesicular sounds on auscultation, his physical examination was unremarkable, with great skin and haircoat.
His overall blood work was totally normal, with the exception of a low serum T4 concentration (0.4 µg/dl; reference range = 0.8-4.0 µg/dl). I added on a free T4 value, expecting it to be normal; however, it was also low at 5 pmol/L (reference range = 10-50 pmol/L).
My question is this: Can the euthyroid sick syndrome can suppress serum T4 and T3 levels in cats, as drugs or disease can do in dogs? I do not feel treatment with levothyroxine (L-T4) is warranted in this cat, but I don't want to ignore low thyroid values either unless I can explain why they might be low.
I'd greatly appreciate your insight on this curious case.
My Response:
I agree with you that Buster would not likely benefit from L-T4 supplementation.
Hypothyroidism is a clinical diagnosis -- if there aren't any clinical signs, the finding of low serum thyroid hormones values alone doesn't justify treatment. This is even more true in cat, where spontaneous hypothyroidism has only been documented in only a couple adults cats. Congenital hypothyroidism in kittens is much more common, but Buster certainly doesn't have congenital hypothyroidism since he is 10 years old!
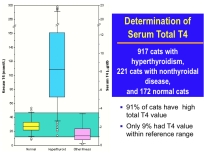
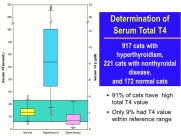
Figure 1: Notice that the total T4 concentrations are low in about half of the cats with nonthyroidal disease (pink box plot on right).
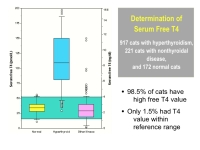
Figure 2: Notice that the free T4 concentrations tend to stay within normal range in cats with nonthyroidal illness (pink box plot on right), but values are subnormal in about 20% of these cats. Also note the falsely "high" values in other sick cats, illustrating some of the problems with the free T4 assay in cats.
It certainly is possible that his asthma and steroid therapy has suppressed both his total and free T4 concentrations. In 2001, I wrote a research paper (1) where we measured total and free T4 in cat with hyperthyroidism and nonthyroridal illness. As you can see in Figures 1 and 2, both total and free T4 were suppressed to low levels in some of the cats who were ill.
Reference:
1. Peterson ME, Melian C, Nichols R. Measurement of serum concentrations of free thyroxine, total thyroxine, and total triiodothyronine in cats with hyperthyroidism and cats with nonthyroidal disease. J Am Vet Med Assoc 2001;218:529-36.
Źródło: endocrinevet.blogspot.com
The dog or cat does not have to be fasted overnight, and lipemia does not appear to “clinically’ affect serum cortisol values. However, having a nonlipemic sample may be better in some situations, especially if serum cholesterol or triglycerides are being measuring on same sample.
Remember that the ACTH stimulation test is the most useful test for monitoring dogs being treated with trilostane (Vetoryl) or mitotane (Lysodren) see my blog entitled, Diagnosing Cushing's disease: Should the ACTH stimulation test ever be used? Both medications are fat-soluble drugs and must be given at time of meals, or the drugs will not be well absorbed.
With trilostane, it’s extremely important to give the morning medication with food, and then start the ACTH stimulation test 3 to 4 hours later.
Fasting these dogs on the morning in which the ACTH stimulation test is scheduled should be avoided since it invalidates the test results.
When a dog ‘s food is withheld, the absorption of trilostane from the gastrointestinal tract is decreased. This leads to low circulating levels of trilostane, resulting in little to no inhibition of adrenocortical synthesis. Therefore, serum cortisol values will higher when the drug is given in a fasted state than when it is given with food.
The higher basal or ACTH-stimulated cortisol results could prompt one to unnecessarily increase the daily trilostane dose. That misjudgment may lead to drug overdosage, with the sequelae of hypoadrenocorticism and adrenal necrosis in some dogs.
Recommended ACTH stimulation test protocol:
 There are many different published protocols for how to perform the ACTH stimulation testing. Both ACTH gel or synthetic ACTH can be used, but over the last 2 decades, the use of cosyntropin (Cortrosyn) has become the “gold standard” preparation for ACTH stimulation testing.
There are many different published protocols for how to perform the ACTH stimulation testing. Both ACTH gel or synthetic ACTH can be used, but over the last 2 decades, the use of cosyntropin (Cortrosyn) has become the “gold standard” preparation for ACTH stimulation testing.In the USA, Cortrosyn is available through Henry Schein (800-872-4346; www.henryschein.com) where it can be purchased as an individual vial ($68/vial) or a box of 10 ($720 per box or 68/vial).
This is the protocol for the Cosyntropin (Cortrosyn) ACTH stimulation test that I recommend:
1. Collect baseline serum or plasma sample for cortisol determination.
Use of a serum separator tube should be acceptable for serum cortisol measurements, but check with your laboratory to ensure proper sample collection.
2. Prepare the ACTH preparation for administration (see below).
Cortrosyn is supplied by the manufacturer as a lyophilized cosyntropin powder in vials containing 0.25 mg (250 µg) of ACTH to be reconstituted with sterile saline solution.
In order to make this test more cost effective when using Cortrosyn and to make it easier to administer this dose to smaller dogs, I recommend diluting the Cortrosyn and dividing the solution into 25-µg to 50-µg aliquots in a tuberculin or insulin syringe, and then refrigerating or freezing the capped syringe.
For specific guideline on how to dilute the Cortrosyn and store it to extend it’s shelf-life, look for may next post entitled: How to extend your supply of Cortrosyn and lower the cost of ACTH stimulation testing.
3. Administer the cosyntropin at a dosage of a 5.0 µg/kg, up to a maximum dose of 250 µg; 1 entire vial).
This 5.0 µg/kg dosage will result in maximum stimulation of the adrenocortical reserve, the most important criteria for any ACTH stimulation protocol.
4. In dogs, the Cortrosyn can be administered either IV or IM, with equivalent cortisol results. Obviously, if the dog is dehydrated or in shock, the Cortrosyn must be administered intravenously.
In cats, its best to administer the Cortrosyn IV, because the adrenocortical response is more consistent and the peak is higher. Given subcutaneously, the Cortrosyn is not well absorbed in cats. In addition, giving Cortrosyn by the IM route is painful for cats and should be avoided.
5. Collect post-ACTH serum sample for cortisol determination 1 hour later.
6. After the clot has retracted, centrifuge both samples.
If using plasma or a serum tube without a separator, aspirate the plasma or serum and transfer into a plastic or glass vial.
Test protocol for tetracosactide (Synacthen):
 If you live in a part of the World other than the USA, it’s likely that you will be using tetracosactide (Synacthen) rather than Cortrosyn as the synthetic ACTH preparation. The chemical structure of tetracosactide and cosyntropin are identical, and the test protocol outlined above will work. However, because the cost of Synacthen is much less than Cortrosyn, it is common practice to administer Synacthen at the dose of a half vial (125 µg) to a cat or small dog and an entire vial (250 µg) to a larger dog, rather use the 5-ug/kg dosage.
If you live in a part of the World other than the USA, it’s likely that you will be using tetracosactide (Synacthen) rather than Cortrosyn as the synthetic ACTH preparation. The chemical structure of tetracosactide and cosyntropin are identical, and the test protocol outlined above will work. However, because the cost of Synacthen is much less than Cortrosyn, it is common practice to administer Synacthen at the dose of a half vial (125 µg) to a cat or small dog and an entire vial (250 µg) to a larger dog, rather use the 5-ug/kg dosage.Źródło: endocrinevet.blogspot.com
Bailey is a 14-year-old male neutered domestic short hair who was diagnosed with hyperthyroidism by another veterinarian about 3 years ago and has been on methimazole since then. He also has a history of chronic constipation that has been well controlled in the last year on enulose (Lactulose) only.
I last saw Bailey a year ago, at which point he was doing well clinically but had lost about 1 lb. since his last check. At that time, he was on 5 mg of methimazole BID. A geriatric profile at that time showed a total T4 of 3.3 µg/dl, a normal CBC and serum chemistry profile (creatinine = 1.5 mg/dl, BUN = 23 mg/dl), and a urine specific gravity of 1.065. I recommended increasing his dose of methimazole to 7.5 mg in the morning and 5 mg in the evening and rechecking in 4-6 weeks.
The owner did increase the daily methimazole dose but did not follow up with us until now. Bailey has lost an additional 3 lbs since July and has developed polyphagia, polyuria and polydipsia over the last month. On exam yesterday, my main physical exam finding was that he now has a fairly large mass in his left ventral neck area (about 3-4 cm, slightly firm and irregular), which I had not noted on the last exam. His blood work from yesterday showed a T4 of 1.9 µg/dl, and very normal renal function (serum creatinine = 1.1 mg/dl; BUN = 22 mg/dl, USG =1.030).
So, I'm suspicious that the thyroid mass is or has become a carcinoma at this point. But would you expect the cat to lose weight secondary to a thyroid carcinoma even if the T4 is within normal range? Could it be secreting another hormone to cause the weight loss?
I thought I should recommend full-body radiographs to try to rule out any metastasis or other obvious neoplasia, and then consider surgical removal and biopsy of the mass. I've read that it can be helpful to follow-up with I131 treatment after excision of a thyroid carcinoma, so I would speak to the owner about referral for that. Does that sound like a reasonable course of action to you or are there other things you would recommend doing first?
Thank you very much for any help or advice you can give me on this cat.
My Response:
There are many ways you could go in your workup of this cat. Most cats that I see who are loosing weight while on treatment with methimazole have high serum T4 concentrations, which can explain the weight loss. Obviously, that's not the case here, which makes this cat more interesting!

Large goiter in hyperthyroid cat
Many cats (in fact, probably nearly all hyperthyroid cats) will have an increase in goiter size with time; that makes sense since we aren't inhibiting thyroid tumor growth with the methimazole. We are only blocking thyroid hormone secretion with the drug.
Recently, a paper was published showing that on thyroid biopsy, some cats with long-standing hyperthyroidism had evidence of transformation of thyroid adenoma to carcinoma. I do believe that this happens more than we realize, and I now see almost a cat a month with thyroid carcinoma. Almost all cats with thyroid carcinoma that I see have been on methimazole for longer than 2 years.
So in your cat, the enlargement of the thyroid mass could indicate that the tumor has simply grown larger with time, or it could indicate malignant transformation. As you indicated, thyroid biopsy would be helpful in making that diagnosis. Many of these cats have extension or metastasis into the thoracic cavity so you might not be able to cure that cat with surgical thyroidectomy if that is the case. What I like to do in that situation is to perform a thyroid scan (thyroid scintigraphy) prior to surgery, which would tell us where the thyroid tumor tissue is located and help direct what needs to be removed or biopsied, if the cat does go to surgery.
That all said, why is your cat loosing weight despite a normal serum T4? With the polyphagia, the cat should be taking in enough calories. If there vomiting or diarrhea? (I am guessing no diarrhea because of the constipation.) Cats with weight loss that are eating normally must have either increased loss of glucose in the urine or impaired absorption of nutrients from the GI tract. To that end, I would recommend that you perform an abdominal ultrasound, in addition to your full-body x-rays, prior to either thyroid biopsy or thyroid scintigraphy. Urine culture should also be considered to exclude pyelonephritis.
As far as other hormones being secreted, I'd suggest that you also measure a serum free T4 and T3 concentration on this cat. It's possible that the serum concentrations of free T4 or T3 are still high and that could explain some of the cat's weight loss.
References:
1) Harvey AM, Hibbert A, Barrett EL, Day MJ, Quiggin AV, Brannan RM, Caney SM. Scintigraphic findings in 120 hyperthyroid cats. J Feline Med Surg. 2009 11:96-106.
Źródło: endocrinevet.blogspot.com









